Which of the following is an example of a hospital-acquired condition when not present on admission?
Which of the following sources provide external benchmarks to examine the effectiveness of a facility's clinical documentation program?
Which entity has the following regulation?
A medical history and physical examination be completed and documented for each patient no more than 30 days before or 24 hours after admission or registration, but
prior to surgery or a procedure requiring anesthesia services.
AHIMA suggests which of the following for an organization to consider as physician response rate and agreement rate?
Whether or not queries should be kept as a permanent part of the medical record is decided by
The clinical documentation integrity (CDI) team in a hospital is initiating a project to change the unacceptable documentation behaviors of some physicians. What
strategy should be part of a project aimed at improving these behaviors?
The most beneficial step to identify post-discharge query opportunities that affect severity of illness, risk of mortality and case weight is to
A clinical documentation integrity practitioner (CDIP) generates a concurrent query and continues to follow retrospectively; however, the coder releases the bill before
the query is answered. The CDIP wonders if it is appropriate to re-bill the account if the physician answers the query after the bill has dropped. Which policy should the
hospital follow to avoid a compliance risk?
A hospital administrator wants to initiate a clinical documentation integrity (CDI) program and has developed a steering committee to identify performance metrics. The
CDI manager expects to use a case mix index as one of the metrics. Which other metric will need to be measured?
Which of the following clinical documentation integrity (CDI) dashboard metrics is frequently used to help evaluate the credibility of CDI practitioner queries and the
success of the CDI program?
A patient was admitted due to possible pneumonia. Chest x-ray was positive for infiltrate. The physician's documentation indicates that the patient continues to smoke
cigarettes despite recommendations to quit. Patient also has a long-term history of chronic obstructive pulmonary disease (COPD) due to smoking. IV antibiotic was
given for pneumonia along with oral Prednisone and Albuterol for COPD.
Discharge diagnoses:
1. Pneumonia
2. COPD
3. Current smoker
What is the correct diagnostic related group assignment?
A patient is admitted for pneumonia with a WBC of 20,000, respiratory rate 20, heart rate 85, and oral temperature 99.0°. On day 2, sputum cultures reveal positive
results for pseudomonas bacteria. The most appropriate action is to
A 94-year-old female patient is admitted with altered mental status and inability to move the left side of her body. She is diagnosed with a cerebral vascular accident with left sided weakness. The patient is ambidextrous, but the physician does not specify the
predominance of the affected side. The default code is
Combination codes are used to classify two diagnoses, a diagnosis with a manifestation, or a diagnosis
Automated registration entries that generate erroneous patient identification—possibly leading to patient safety and quality of care issues, enabling fraudulent activity involving patient identity theft, or providing unjustified care for profit—is an example of a potential breach of:
The BEST place for the provider to document a query response is which of the following?
Which of the following is used to measure the impact of a clinical documentation integrity (CDI) program on Centers for Medicare and Medicaid Services quality performance?
Which factors are important to include when refocusing the primary vision of a clinical documentation integrity (CDI) program?
A 56-year-old male patient complains of feeling fatigued, has nausea & vomiting, swelling in both legs. Patient has history of chronic kidney disease (CKD) stage III,
coronary artery disease (CAD) & hypertension (HTN). He is on Lisinopril. Vital signs: BP 160/80, P 84, R 20, T 100.OF. Labs: WBC 11.5 with 76% segs, GFR 45. CXR
showed slight left lower lobe haziness. Patient was admitted for acute kidney injury (AKI) with acute tubular necrosis (ATN). He was scheduled for hemodialysis the
next day. Two days after admission patient started coughing, fever of 101.8F, CXR showed left lower lobe infiltrate, possible pneumonia. Attending physician
documented that patient has pneumonia and ordered Rocephin IV. How should the clinical documentation integrity practitioner (CDIP) interact with the physician to
clarify whether or not the pneumonia is a hospital-acquired condition (HAC)?
A 27-year-old male patient presents to the emergency room with crampy, right lower quadrant abdominal pain, a low-grade fever (101° Fahrenheit) and vomiting. The
patient also has a history of type I diabetes mellitus. A complete blood count reveals mild leukocytosis (13,000/microliter). Abdominal ultrasound is ordered, and the
patient is admitted for laparoscopic surgery. The patient is given an injection of neutral protamine Hagedorn insulin, in order to normalize the blood sugar level prior to
surgery. Upon discharge, the attending physician documents "right lower quadrant abdominal pain due to possible acute appendicitis or probable Meckel diverticulitis".
What is the proper sequencing of the principal and secondary diagnoses?
An otherwise healthy male was admitted to undergo a total hip replacement as treatment for ongoing primary osteoarthritis of the right hip. During the post-operative
period, the patient choked on liquids which resulted in aspiration pneumonia as shown on chest x-ray. Intravenous antibiotics were administered, and the pneumonia was
monitored for improvement with two additional chest x-rays. The patient was discharged to home in stable condition on post-operative day 5.
Final Diagnoses:
1. Primary osteoarthritis of right hip status post uncomplicated total hip replacement
2. Aspiration pneumonia due to choking on liquid episode
What is the correct diagnostic related group assignment?
For inpatients with a discharge principal diagnosis of acute myocardial infarction, aspirin must be taken within 24 hours of arrival unless a contraindication to aspirin is
documented. How should this be documented in the health record?
A patient presented with shortness of breath, elevated B-type natriuretic peptide, and lower extremity edema to the emergency room. During the hospitalization, a cardiac
echocardiogram was performed and revealed an ejection fraction of 55% with diastolic dysfunction. The patient's history includes hypertension (HTN), chronic kidney
disease (CKD) (baseline glomerular filtration rate 40) and congestive heart failure (CHF). The clinical documentation integrity practitioner (CDIP) has queried the
physician to further clarify the patient's diagnosis. Which response provides the highest level of specificity?
Which of these medical conditions would a clinical documentation integrity practitioner (CDIP) expect to be treated with Levophed?
A hospital clinical documentation integrity (CDI) director suspects physicians are over-using electronic copy and paste in patient records, a practice that increases the
risk of fraudulent insurance billings. A documentation integrity project may be needed. What is the first step the CDI director should take?
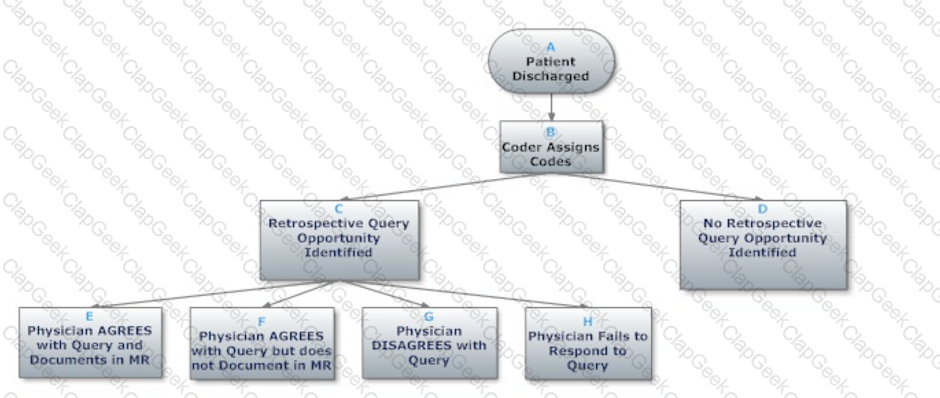
Based on the flowchart below, at what point might the clinical documentation integrity practitioner (CDIP) enlist the help of the physician advisor/champion?
A patient was admitted with complaints of confusion, weakness, and slurred speech. A CT of the head and MRI were performed and resulted in normal findings. Daily
aspirin was administered and a speech therapy evaluation was conducted. The final diagnosis on discharge was transient ischemic attack, and cerebrovascular disease
was ruled out. What is the correct diagnostic related group assignment?
A clinical documentation integrity practitioner (CDIP) is looking for clarity on whether a diagnosis has been "ruled in" or "ruled out". Which type of query is the best option?
Which of the following may make physicians lose respect for clinical documentation integrity (CDI) efforts and disengage?
The clinical documentation integrity (CDI) manager has noted a query response rate of 60%. The CDI practitioner reports that physicians often respond verbally to the
query. What can be done to improve this rate?
While reviewing a chart, a clinical documentation integrity practitioner (CDIP) needs to access the general rules for the ICD-10-CM Includes Notes and Excludes Notes
1 and 2. Which coding reference should be used?
A 50-year-old male patient was admitted with complaint of 3-day history of shortness of breath. Vital signs: BP 165/90, P 90, T 99.9.F, O2 sat 95% on room air. Patient
has history of asthma, chronic obstructive pulmonary disease (COPD), and hypertension (HTN). His medicines are Albuterol and Norvasc. CXR showed chronic lung
disease and left lower lobe infiltrate. Labs: WBC 9.5 with 65% segs. Physician documented that patient has asthma flair and admitted with decompensated COPD,
ordered IV steroids, O2 at 2L/min via nasal cannula, Albuterol inhalers 4x per day, and Clindamycin. Patient improved and was discharged 3 days later. Which action
would have the highest impact on the patient's severity of illness (SOI) and risk of mortality (ROM)?
Review the following query to determine if it is compliant:
Dr. Jones, this patient had a sodium level of 126 on admission and was started on a 0.9% saline IV. Can you indicate what condition is being treated?
Dehydration
Hyponatremia
Hypernatremia
Chronic kidney disease (indicate stage)
Other (please specify)
A patient receives a blood transfusion after a 400 ml blood loss during surgery. The clinical documentation integrity practitioner (CDIP) queries the physician for an
associated diagnosis. The facility does not maintain queries as part of the permanent health record. What does the physician need to document for the CDIP to record the
query as answered and agreed?
A patient presents to the emergency room with acute shortness of breath. The patient has a history of lung cancer that has been treated previously with radiation and
chemotherapy. The patient is intubated and placed on mechanical ventilation. A chest x-ray is remarkable for a pleural effusion. A thoracentesis is performed, and the
cytology results show malignant cells. Diagnoses on discharge: Acute respiratory failure due to recurrence of small cell carcinoma and malignant pleural effusion. Which
coding reference takes precedence for assigning the ICD-10-CM/PCS codes?